Wondering if HRT is for you? As newer forms of hormone replacement therapy arrive, we take a closer look at the pros and cons of the treatment, including the benefits of HRT for relieving menopause symptoms alongside the risks and side effects…
New medicines have been transformative for women’s health. Hormone replacement therapy (HRT) changed menopause from a life stage to suffer through in silence, to one in which you could feel as energised as ever. For years HRT was seen as a wonder drug for women’s health and was one of the world’s most prescribed medications. That is until the end of last century, when the controversy surrounding the risks began…
What is hormone replacement therapy?
The main hormone responsible for the changes occurring at the menopause is oestrogen. One of the primary aims of HRT is restoring oestrogen to a level that is sufficient to minimise menopausal symptoms.
In women who have a uterus, progesterone is also necessary to keep the endometrium healthy and avoid any thickening, which can be caused by taking oestrogen on its own. Combined HRT replenishes oestrogen and progestogen hormones, which naturally decline in the lead up to menopause, with synthetic versions, to relieve menopause symptoms.
Should I try hormone replacement therapy for menopause relief?
Hormone replacement therapy is an effective way to reduce the severity of, or even prevent, many common but what can be debilitating symptoms. This includes hot flushes, night sweats and joint aches, to helping with insomnia, brain fog and anxiety.
Hormone replacement therapy can also provide major health benefits for both your bones and heart. Taking HRT long term can help maintain bone density and reduce the risk of osteoporosis. It can also reduce the risk of heart disease and stroke.
How do I ask my doctor for hormone replacement therapy?
If you are considering a consultation with your GP, attend fully prepared. Unfortunately, many doctors are not fully up to date with current HRT research. This can lead to doctors offering women incorrect advice. If you feel this is the case, ask for a second opinion.
Alternatively, you can ask to be referred to an accredited menopause specialist. Similarly, if you feel your HRT prescription does not suit you, look at different types or strengths of HRT. Often, you’ll need to frequently “tweak” hormones. It can also take four to six months to optimise the regime and control your menopausal symptoms.

Benefits of hormone replacement therapy
The most immediate and visible effect of HRT is that it can stop or reduce physical and psychological menopausal symptoms. Taking HRT has also been proven to prevent and stabilise the bone loss that occurs due to age and declining oestrogen at the menopause. This is true even when HRT is taken at a low dosage.
While there has been debate about whether HRT is good for the heart or potentially harmful, HRT taken ideally within 18 months of the menopause can reduce your risk of developing cardiovascular disease. Timing is key, and evidence points to a “cardiovascular window of opportunity”. This is ideally within 10 years of the menopause.
Research has also found that oestrogen can maintain lower overall cholesterol levels. Regarding Alzheimer’s disease, there is conflicting research. However, there is some evidence that HRT may help reduce the risk of Alzheimer’s and other forms of dementia. In terms of long-term health, HRT can help with weight management and muscle retention. It may even help delay the onset of Type 2 diabetes.
Are newer forms of HRT better?
Many women remain worried about the potential risks of HRT. But nowadays modern body-identical hormones have transformed the role of HRT during the menopause. In fact, current research is showing that taking the newer forms of HRT and starting treatment earlier, at the transition to menopause, can either reduce or eliminate these risks.
Most information leaflets accompanying HRT prescriptions include a long list of potential cautions which you should consider before commencing treatment. Unfortunately, much of this information is outdated.
Many of the risks have been overblown or disproven and may have changed due to the availability of newer and improved versions of HRT. While HRT is generally safe and beneficial for most women, it is important to understand the pros and cons of treatment. This will allow you to make a balanced decision about whether it is the right choice for you.
What is bioidentical HRT?
Today, you can take bioidentical (or ‘body-identical’) HRT, from plant sources, which is available from the NHS. ‘Regulated bioidentical hormones have exactly the same chemical structure as the hormones your ovaries would have produced. Because they’re bioidentical, your body tends to tolerate them better with fewer side effects,’ says NHS gynaecologist Nick Panay, who is also on the medical advisory committee of the British Menopausal Society.
A common misconception is that older types of HRT are synthetic, so must be harmful, whereas bioidentical ones are natural, therefore better. In fact, both types are synthesised and both have similar benefits and risks. To make regulated bioidentical hormones, a chemical is extracted from yams and soy. It’s then synthesised in a lab to create oestrogen, progesterone and testosterone. Older types of HRT are similar to your hormones but are not exactly the same. Some are derived from animal sources, others are created from chemicals.
‘Some research suggests regulated bioidentical progesterone is gentler on breast tissue as it doesn’t stimulate it as much as some synthetic types of progesterone (over-stimulation could trigger cancer). However, every woman responds to hormone therapy differently, so regulated bioidentical hormones might not suit everyone, which is when synthetics might be used,’ says Nick, who directs women’s health clinics at Chelsea & Westminster NHS Hospital and Queen Charlotte NHS hospital.
‘Each woman’s individual risks, such as weight, age and health, need to be assessed before taking HRT. And I always suggest trying lifestyle changes to improve menopause symptoms before using HRT: improving diet, exercising, stopping smoking, and minimising alcohol and caffeine,’ Nick adds.

What are the risks of HRT?
Many women have had concerns about using hormone replacement therapy (HRT). But nowadays modern body-identical hormones have transformed the role of HRT during the menopause. While there are many potential benefits to HRT, there are also a couple of potential risks you should consider.
Despite being used successfully for decades, HRT has gotten a bit of a bad rep due to the risks associated with it. In 2002, a US-based Women’s Health Initiative study (WHI) reported a significant risk of death from breast and ovarian cancer, heart attack and blood clots in women using HRT.
The study followed about 17,000 postmenopausal women aged 50-79 who were taking oestrogen and progestin (a synthetic progesterone). These shocking findings were strengthened by the results of a huge study from the University of Oxford, called The Million Women Study. This analysed data from 1.3 million UK women aged 50 and over, between 1996 and 2001. It found combined HRT users were at twice the risk of breast cancer than non-users.
Are these findings accurate?
Unsurprisingly, these results caused panic and requests for HRT dropped sharply; by 2013, only five per cent of women in the UK were using HRT. But the latest thinking challenges this apparently damning evidence, suggesting previous studies were misleading and their results premature.
An 18-year follow-up of patients in the WHI study, published in 2017, found women aged 50-59 who took HRT had a lower mortality rate than the control group. So, in a remarkable reversal, the most up-to-date finding from this study is that HRT does not cause higher mortality from any cause.
The Million Women study has also been criticised for having structural flaws. This is namely because it was an observational survey rather than a more rigorous, randomised trial. In 2015, the Department of Health’s National Institute for Health and Care Excellence (NICE) came out in favour of HRT. The organisation published guidance, saying HRT works and should be offered to menopausal women.






Does HRT cause breast cancer?
The risk of breast cancer is often the one that concerns women the most when starting HRT. This is understandable as there has been widespread coverage in the media. However, this does not accurately reflect the entire literature on the subject. Plus, breast cancer is very common. This makes it harder to determine what the underlying cause is in any one case.
Oestrogen alone has not been shown to increase the risk of breast cancer. However, the data about progestogens and breast cancer is more mixed. It is thought that the real risk lies in women on combined HRT, taking both oestrogen and progestogen. Of key importance, the newer and increasingly used body-identical micronised progesterone has impressive data. This shows its safety as far as breast cancer is concerned.
Can HRT increase risks of blood clots?
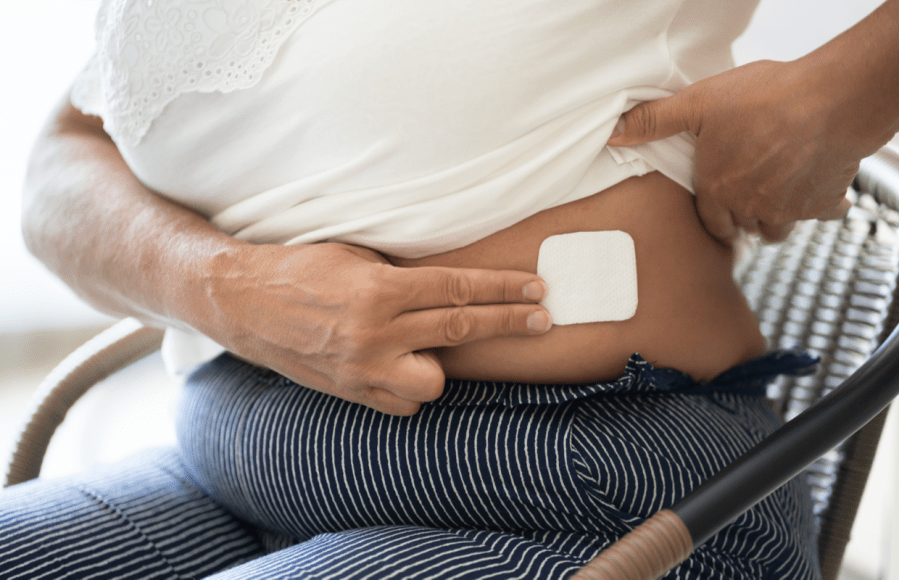
Oestrogen as a hormone is associated with an increased risk of forming blood clots. This is true even of the oestrogen your body creates. Oral forms of HRT including oestrogen are associated with a very small but definite increase in the risk of blood clots. However, this is not the case with bioidentical oestrogen that you apply transdermally to the skin, such as patches, gels, or sprays, so are a safer option.
What are the side effects of hormone replacement therapy?
Most side effects tend to resolve with time, particularly after six to eight weeks of starting HRT. Some women can experience mastalgia (breast tenderness), abdominal bloating and headaches. Some of these may be dose-related. Therefore, you can minimise these symptoms by starting HRT cautiously and building up the dose.
In women with a uterus, unscheduled vaginal bleeding can happen in as many as 40 per cent of women. This usually occurs in the first four to six months of treatment. However, this should not cause alarm in most cases. A surprising number of women are also relatively intolerant to progestogens. These women can develop symptoms that are similar to PMS. Fortunately, these tend to subside with time.
As mentioned previously, most people’s bodies tolerate the newer bioidentical forms of HRT better, meaning they experience fewer side effects. Consider asking your doctor about these newer, plant-based forms of the treatment if you are struggling with the side effects of HRT.
Is HRT worth the health risks?
Doctors in general conclude that women experiencing menopause symptoms can benefit from regulated HRT. And, in most cases, the benefits of HRT outweigh the risks. Women who can benefit from HRT includes women in perimenopause, usually from mid-to-late 40s, who are still menstruating but can have symptoms as hormone levels begin to drop.
Postmenopausal women, whose last period was more than a year ago, can also benefit. This is because, on average, symptoms of menopause can continue for three to five years. They also say the risks of original HRT and regulated bioidentical HRT are thought to be very similar at present.
According to NICE there’s no additional risk of breast cancer if you’re on combined HRT and are under 50 years old. For women above 50, in every 1,000 women taking combined HRT there will be about four more cases of breast cancer than in women not taking it. Women over 60 on HRT have a slightly increased risk of cardiovascular disease and stroke.
There is also a risk of deep vein thrombosis (DVT) from all types of HRT. However, your level of risk depends upon other factors, such as weight, age and whether or not you smoke. It’s worth noting the risk of DVT from HRT is lower than it is for women on the contraceptive pill and during pregnancy.
How to lower the risks of HRT:
You can lower the risks associated with HRT by using gel or patches rather than pills, as the hormones go directly into the blood, rather than your stomach and liver having to process them. Taking oestrogen-only HRT can also cause womb cancer. This is why doctors usually recommend combined HRT, as progesterone balances out oestrogen, preventing it from over-thickening womb walls, which can trigger cancer.
Lastly, if your GP doesn’t have up-to-date info on HRT or refuses to prescribe it, you have the right to see another GP. And you can seek advice from the charity Women’s Health Concern, which is the patient branch of the British Menopause Society.
You can find out more about hormone replacement therapy and other treatment options for the menopause in Natural Menopause: Herbal Remedies, Aromatherapy, CBT, Nutrition, Exercise, HRT for Perimenopause, Menopause, and Beyond, by consultant editor, Anne Henderson (£14.99).
Related: 8 tips to enjoy great sex after the menopause
Words: Dr Anne Henderson and Angela Kennedy | Images: Shutterstock